Brain surgery and augmented reality - it sounds like something that is likely being used at the Mayo Clinic, or a University Hospital in a major metropolis. But, St. Luke’s Boise has recently implemented this cutting edge technology and they’re one of the first in the nation to do so. We recently had the chance to meet with Dr. Edward Duckworth who is the St. Luke’s Director of Neurosurgery to learn more about this technology and how it’s being used.
As is often the case, good timing played a part into why they brought this technology to the operating room. The hospital was in the process of looking at a microscope upgrade, and was committed to having the latest in microscope technology. St. Luke’s was the first in the country (Dr. Duckworth argues the world!) to obtain the latest Zeiss microscope called the Kinevo. Brainlab, also a German company, worked with Zeiss to design an integrated image guidance platform that incorporates augmented reality. Seeking to build a world class brain surgery program, the hospital realized it made sense to take the technology to the next level.
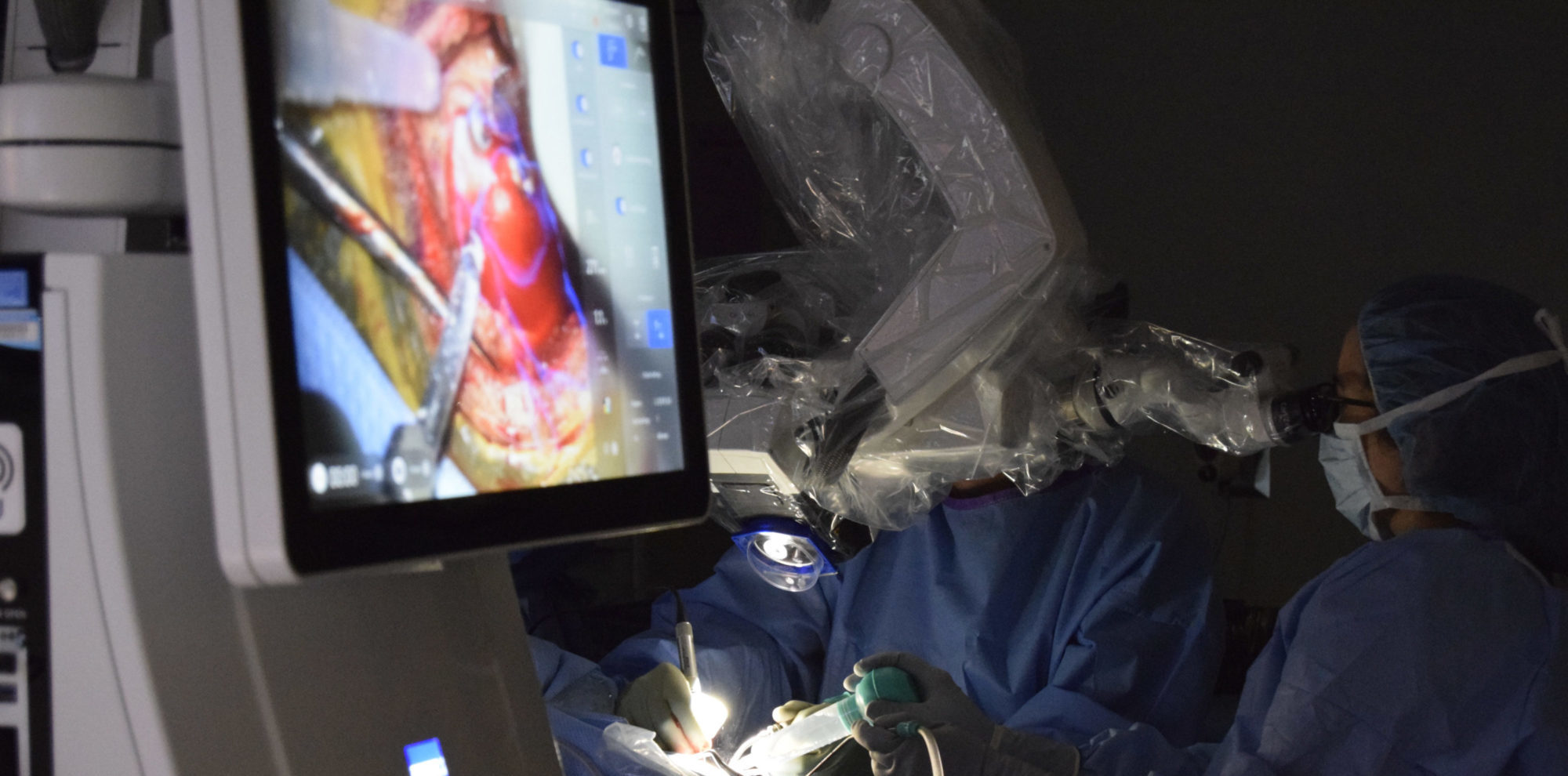
Augmented reality brain surgery utilizes advanced preoperative imaging (typically MRI), the microscope, the navigation system, and sometimes intraoperative imaging (ultrasound) as well. The idea is that the surgeon is able to visualize the planned surgical target and surrounding structures as semi-transparent volumes mixed with the anatomy seen, providing better spatial orientation throughout the procedure. Critical structures, such as important fiber tracts, can be highlighted.

Using AR During Surgery
Dr. Duckworth states that AR is the logical evolution of technological assistance in the O.R. Neurosurgery technical advancements have evolved from the emergence of basic image guidance 20-30 years ago, to the microscope talking to the image system 10-15 years ago, and now augmented reality is arguably a paradigm shift, with the overlaying of data in the microscope. Prior to even getting into the OR though, the technology is allowing for better pre-surgery planning. Surgeons can visualize what fiber tracts or functional areas (motor or speech, eg.) are relevant to the patient’s pathology, and choose an approach which will minimize the risks to these structures. From a patient perspective, imagine being able to come in and see your brain with AR overlay of the pathology, whether it be a tumor or vascular malformation, and a simulation of of exactly what the surgery will look like. This can now be done, and they are hoping this experience will decrease patient anxiety regarding their upcoming surgery. Once in the operating room, the surgeon can see critical anatomy, the target lesion (eg. Tumor) under the surface, and the relevant fiber tracks with AR overlay within the eyepieces of the microscope or on a 3D 4K large monitor within the room. While there is no substitute for the years of training it takes to be a cranial neurosurgeon (12 years after college), Dr. Duckworth says there is no amount of education that can give you that type of real time understanding.
After using AR in approximately 40 surgeries Dr. Duckworth says enthusiastically that he never wants to go back to the old way of operating! He says it’s like giving the surgeon X-Ray vision. WOW! We’re excited to see this cutting edge technology right here in Idaho. Thank you to St. Luke’s, Northwest Neurosurgery Associates and Dr. Duckworth for sharing their journey into AR with us. If you have any questions or want any more information regarding “Augmented Reality Brain Surgery”, please contact Ben Slee, the St. Luke's Health System Cranial program manager, at sleeb(at)slhs.org.

Recent Comments